IgG4-related disease
OVERVIEW
What is IgG4-related disease?
IgG4-related disease was formally named by Japanese scholars in 2010. Current research suggests it is a broad category of chronic immune-mediated fibroinflammatory disorders that can cause lesions in multiple organs, with varying effects on patients depending on the affected organs.
Patients often present with mass formation in the affected organs (e.g., orbital pseudotumor, kidney masses resembling renal cell carcinoma, or nodular lung lesions) or diffuse organ enlargement (e.g., pancreatic swelling).
Most patients have multiple affected organs. The disease is very rare and predominantly occurs in middle-aged and elderly men.
Glucocorticoids are the first-line treatment for this condition. Most patients respond well to treatment, but regular monitoring is required after dose reduction or discontinuation to prevent relapse.
What are the common types of IgG4-related disease?
-
Type 1 (IgG4-related) autoimmune pancreatitis: IgG4-related sclerosing cholangitis, often co-occurring with type 1 autoimmune pancreatitis.
-
Major salivary gland enlargement or sclerosing sialadenitis: When lacrimal, parotid, and submandibular gland enlargement occur together, it is termed IgG4-related Mikulicz disease.
-
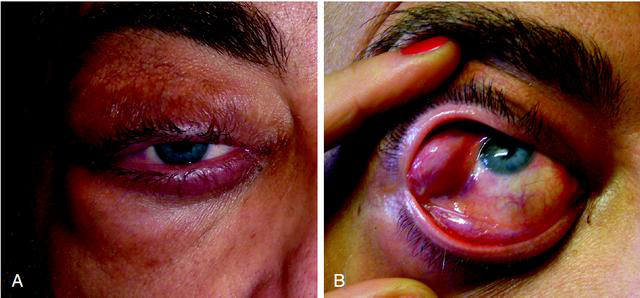
Orbital disease: Often accompanied by proptosis.
-
Retroperitoneal fibrosis: Frequently associated with chronic periaortitis, often involving the ureters, leading to hydronephrosis and kidney damage.
Affected organs share key features and prominent manifestations, collectively referred to as IgG4-related disease.
Is IgG4-related disease common?
The exact prevalence of IgG4-related disease remains unknown, partly due to its late recognition in the medical community. The first international expert consensus on diagnosis and treatment was not established until 2015.
This disease is extremely rare in China and is listed in the country's First Catalog of Rare Diseases. It predominantly affects middle-aged and elderly men. Due to its frequent presentation as mass-like lesions, it is often misdiagnosed as malignancy. No specific incidence data is available from Chinese studies.
SYMPTOMS
What are the symptoms and manifestations of type 1 autoimmune pancreatitis (AIP) in IgG4-related diseases?
Autoimmune pancreatitis (AIP) is a rare condition. Current research classifies AIP into two major types, with the IgG4-related type being type 1, which accounts for the vast majority of AIP cases. The characteristic symptoms of type 1 AIP include:
-
Pancreatic mass: May mimic pancreatic cancer or lymphoma, often accompanied by pancreatic duct strictures.
-
Mild abdominal pain: Sometimes associated with acute or chronic pancreatitis.
-
Biliary manifestations: Details are discussed in the next question.
-
Diabetes
What are the symptoms and manifestations of sclerosing cholangitis in IgG4-related diseases?
Unlike primary sclerosing cholangitis, tissue biopsy in IgG4-related cholangitis patients reveals IgG4+ plasma cell infiltration and severe interstitial fibrosis. Patients may exhibit elevated serum IgG4 levels and a characteristic response to glucocorticoids.
It typically occurs alongside type 1 AIP and rarely appears alone. Main manifestations include bile duct strictures, obstructive jaundice (yellowing of the eyes and skin, dark urine, pale stools). Liver function tests show obstructive jaundice, significantly elevated serum alkaline phosphatase, and mildly elevated liver transaminases.
What are the symptoms and manifestations when IgG4-related diseases affect the salivary and lacrimal glands?
Manifestations include swelling of the lacrimal and parotid glands, as well as submandibular glands, leading to mild dry mouth and dry eyes.

What are the symptoms and manifestations of IgG4-related dacryoadenitis and orbital inflammatory lesions?
The lacrimal glands, eyeballs, and orbits are often affected alongside the salivary glands. Dry mouth from salivary gland involvement is mild, and dry eyes from lacrimal gland involvement are also mild. However, lacrimal gland swelling and orbital pseudotumors are common.
What are the symptoms and manifestations of retroperitoneal fibrosis and related conditions in IgG4-related diseases?
IgG4-related disease patients may develop chronic peritoneal inflammation and fibrosis, affecting surrounding tissues—for example, causing obstructive uropathy by compressing the ureters. It also frequently involves the infrarenal abdominal aorta and extends to the bilateral iliac arteries.
Other manifestations include sclerosing mesenteritis, sclerosing mediastinitis, and multifocal fibrosclerosis.


What are the symptoms and manifestations of aortitis and periaortitis in IgG4-related diseases?
In addition to retroperitoneal fibrosis encasing the abdominal aorta, non-infectious thoracic or abdominal aortitis may occur, characterized by vascular wall inflammation, perivascular tissue inflammation, and possible arterial lumen dilation.
What are the manifestations of other organ involvement in IgG4-related diseases?
Other organ lesions often accompany the commonly affected organs mentioned above.
-
Thyroid involvement: May lead to Riedel’s thyroiditis, presenting as a hard thyroid goiter and causing compression-related symptoms (e.g., dyspnea, dysphagia, hoarseness).
-
Lung and pleural involvement: May manifest as cough, hemoptysis, dyspnea, pleuritis, or chest pain, or may be asymptomatic. Chest CT findings include:
- Solid nodules;
- Bronchovascular pattern (with thickening of bronchovascular bundles and interlobular septa);
- Alveolar interstitial pattern (with honeycombing, bronchiectasis, and diffuse ground-glass opacities);
- Round, ground-glass opacities.
-
Kidney involvement: Typically occurs alongside other organ involvement. Manifestations include abnormal urinalysis and renal insufficiency. Pathologically, it presents as tubulointerstitial nephritis (TIN), with a minority showing mild mesangial proliferative glomerulonephritis, membranous nephropathy, or focal segmental intracapillary hypercellularity.
-
Skin involvement: Papules, plaques, and nodules are common cutaneous manifestations, rarely presenting as macules or bullae. Predominantly affects the head, neck, and auricular skin.
-
Central nervous system involvement: The most common manifestations are hypopituitarism due to IgG4-related hypophysitis and hypertrophic pachymeningitis.
-
Others: Includes liver disease, constrictive pericarditis, lymphoplasmacytic gastritis, sclerosing mastitis and breast inflammatory pseudotumors, prostatitis, ovarian lesions, nasopharyngeal lesions, etc.
CAUSES
What is the pathogenesis of IgG4-related disease?
The exact pathogenesis of this disease remains incompletely understood, but increasing evidence suggests:
-
It is an autoimmune disorder in which T cells, particularly CD4+ and follicular helper T (Tfh) cells, play a significant role.
-
IgG4 itself is not pathogenic but rather an immune response to the underlying condition.
-
Elevated serum and tissue IgG4 levels are observed in many diseases, such as multicentric Castleman disease, allergic disorders, eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome), and sarcoidosis.
Therefore, neither elevated serum IgG4 nor histopathological IgG4 positivity alone is sufficient to confirm a diagnosis of IgG4-related disease.
In summary, IgG4 elevation is a secondary phenomenon rather than a driving factor of the disease.
What are the causes of IgG4-related disease?
The etiology of this disease remains unclear but may involve genetic predisposition, microbial infections, and abnormal autoimmune responses. Current research suggests it is a chronic immune-mediated fibroinflammatory disorder capable of affecting multiple organs.
DIAGNOSIS
How is IgG4-related disease diagnosed?
1. Medical history and physical examination:
During diagnosis, doctors carefully review the patient's medical history (previous conditions) and conduct a physical examination before considering the possibility of IgG4-related disease. It is inappropriate to suspect this disease solely based on elevated serum or histopathological IgG4 levels without supporting medical history or clinical signs.
2. Serum IgG4 testing:
Elevated serum IgG4 is a key diagnostic marker and one of the diagnostic criteria for IgG4-related disease. Studies show that increased serum IgG4 levels correlate with the number of affected organs—meaning the more severe the disease, the higher the serum IgG4 levels.
However, elevated serum IgG4 is not highly specific. Many conditions can cause IgG4 elevation, and in most cases without screening, IgG4-related disease is not the cause.
Additionally, a proportion of IgG4-related disease patients do not exhibit significantly elevated serum IgG4 levels.
Therefore, doctors must not rely solely on blood test results but should combine symptoms and clinical signs for diagnosis.
3. Histopathological examination:
Generally, a definitive diagnosis of IgG4-related disease requires histopathological evidence to rule out malignancies and similar conditions. The histopathological features of IgG4-related disease include:
-
Dense lymphoplasmacytic infiltration with fibrosis.
-
IgG4+ plasma cells accounting for >40% of IgG+ plasma cells, with >10 IgG4+ plasma cells per high-power field.
-
Storiform fibrosis and obliterative phlebitis, which enhance diagnostic specificity.
4. Imaging studies:
-
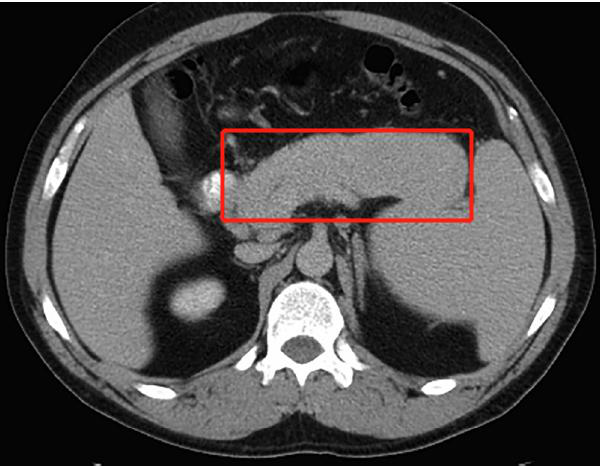
Autoimmune pancreatitis typically shows diffuse pancreatic enlargement with a sausage-like appearance.
-
Retroperitoneal fibrosis presents as soft tissue masses surrounding arteries.
-
Sclerosing cholangitis manifests as thickened bile duct walls with irregular, beaded strictures.
-
Central nervous system involvement may include diffuse pituitary enlargement or hypertrophic pachymeningitis.
What diseases should IgG4-related disease be differentiated from?
Differential diagnosis for conditions with significant IgG4+ plasma cell infiltration:
-
ANCA-associated vasculitis (primarily eosinophilic granulomatosis with polyangiitis).
-
Peritumoral infiltration in adenocarcinomas and squamous cell carcinomas.
-
Multicentric or localized Castleman disease.
-
Lymphoproliferative disorders.
-
Rosai-Dorfman disease.
-
Primary sclerosing cholangitis.
Organ-specific differential diagnoses:
-
Pancreas: Differentiate from pancreatic cancer, other pancreatitis types, and type 2 AIP.
-
Bile ducts: Differentiate from cholangiocarcinoma, primary biliary cholangitis, and primary sclerosing cholangitis.
-
Eyes/orbit: Differentiate from Sjögren’s syndrome.
-
Lymphadenopathy: Differentiate from Castleman disease and other lymphoproliferative disorders.
-
Retroperitoneal fibrosis: Differentiate from idiopathic retroperitoneal fibrosis.
The more thorough the differential diagnosis, the higher the diagnostic reliability and the easier it is to confirm the disease.
Imaging techniques such as CT, PET, MRI, MR cholangiopancreatography, and endoscopic ultrasound provide essential information for diagnosis and differential diagnosis.
TREATMENT
Which department should patients with IgG4-related diseases visit?
Rheumatology and Immunology.
How should IgG4-related diseases be treated?
Glucocorticoids are currently the first-line treatment for IgG4-related diseases, to which patients generally respond well. However, some patients may struggle with dose reduction after improvement.
If disease relapse occurs during gradual tapering or low-dose maintenance therapy, rituximab may be considered as an add-on treatment.
If rituximab is not an option, azathioprine or mycophenolate mofetil can be used instead.
During treatment, monitor the patient's serum IgG4 levels, complement levels, eosinophils, IgE levels, vital organ function, and imaging changes.
DIET & LIFESTYLE
What should patients with IgG4-related disease pay attention to in their daily lives?
IgG4-related disease is a rare condition, and many aspects remain unclear. Generally, standard health measures are recommended, with no special requirements.
What dietary precautions should patients with IgG4-related disease take?
If IgG4-related disease involves digestive organs such as the pancreas or bile ducts, specific dietary considerations may apply (see related conditions for details). For other IgG4-related disease patients, there are no special dietary restrictions—maintaining a healthy, balanced diet is sufficient.
PREVENTION
Can IgG4-related diseases be prevented?
The pathogenesis of IgG4-related diseases is not yet fully understood, and there are currently no effective preventive measures.